Does Hormone Replacement Therapy (HRT) Really Cause Cancer?
Written by Dr. Natalie Barriball
Does HRT cause or increase the risk of cancer?
In short, no, HRT does not cause cancer when used appropriately. Synthetic progesterones (progestins) and unopposed estrogen in women with a uterus are the only hormones shown to increase cancer risk, while other forms of HRT, when dosed correctly, show no increased risk of cancer and may even carry a decreased risk for some cancers. However, it is important to consider the forms, dosing, and individual risk factors when considering overall cancer risk related to hormone therapy.
This risk can depend on (1):
Which hormones are used. Unopposed estrogen has a higher risk of causing endometrial cancer than estrogen and progesterone together.
How they are administered (oral, transdermal, vaginal, etc.). Oral estrogen has more risk factors associated with it, including blood clots, compared to transdermal (topical) estrogen.
The dose used. Higher dosages above physiologic levels can increase tissue growth, which in turn increases the risk of abnormal cells, or cancer cells, developing.
Individual risk factors. Age, genetics, and comorbidities can all contribute to higher or lower individual risk for cancer, with or without HRT.
Synthetic vs Bioidentical
Synthetic hormones have a different molecular structure compared to the hormone molecules our bodies make, which allows them to be much more potent. Synthetic hormones are most commonly seen in birth control products, as the potentiated form allows shutting off of reproductive functions, resulting in contraception. Synthetic hormones are frequently used for hormone replacement in menopause, but are progressively falling out of favor due to higher associations with cancer and blood clot risk. There is also standardized dosing, making it better regulated by the FDA but more difficult to individualize.
Bioidentical hormones are increasing in popularity due to their lower risk and side effect profile. These hormones, as the word implies, are identical to the molecular structure of the body’s hormones. They bind hormone receptors in the same way and to the same effect. This makes them a true “replacement” for the hormones being lost during aging. They are considered safer because of this and are better tolerated by the body. Many forms of bioidentical hormones can be custom-compounded to fit an individual patient. The main criticisms are less regulation by the FDA and less established research.
Most research on cancer and HRT risk is done on synthetic hormones, rather than bioidentical, making the risk difference between the two unclear. Bioidenticals are often considered to have lower risks than synthetic hormones; however, more research is required to establish a true risk assessment. The majority of the research below is on synthetic hormones unless otherwise stated. But as you’ll see, even synthetic hormones are not considered to have a high cancer risk, meaning bioidentical hormones will likely have even lower risk. Hopefully, research in the coming years will shine light on this area.
Types of Cancers and Risk with HRT
Breast Cancer
Summary: Breast cancer risk is only increased by synthetic estrogen combined with synthetic progesterone. Estrogen with micronized progesterone (bioidentical) mitigates this risk and may even lower the overall risk of breast cancer. Testosterone may protect against breast cancer.
The Women’s Health Initiative (WHI) study done between 1993 and 2005 is the study often cited as showing a correlation between HRT and breast cancer. However, recent closer inspection of the study revealed that only synthetic estrogen plus synthetic progestin resulted in a slight increase (1.24-1.28 times) in breast cancer risk after 3-5 years on therapy. And estrogen alone (in women without a uterus) did not increase the risk of breast cancer and may even slightly lower it. This all concludes that only synthetic progesterone (not estrogen or bioidentical progesterone) may very slightly increase breast cancer risk (2, 3).
Other observational studies show there may be an increased risk of breast cancer with the use of unopposed estrogen. However, when estrogen is combined with micronized progesterone, not only is the increased risk mitigated, but the overall risk of breast cancer is actually decreased (4, 5, 6, 7, 8).
While often forgotten about in women, the limited studies on testosterone use in females show its use may actually have a protective effect against breast cancer (9).
Research is limited on the use of bioidentical hormones, but preliminary studies show bioidentical estradiol, estriol, and progesterone lower the overall risk of breast cancer compared to those who have never used HRT (10).
Endometrial Cancer
Studies show that estrogen alone (unopposed estrogen) increases the risk of endometrial cancer if the uterus has not been removed. Adding adequate bioidentical progesterone eliminates this risk (11).
Ovarian Cancer
Synthetic estrogen alone increases the risk of ovarian cancer, but when combined with synthetic progesterone, the risk is not increased and may even be reduced. This does not consider the use of bioidentical hormones, for which there are no studies. But given that bioidenticals are generally considered safer than synthetic, if there are no risks with combined synthetic HRT, there is likely no risk associated with combined BHRT either (12).
Colorectal Cancer
Research shows that there may be a slightly decreased risk of colorectal cancer in HRT users.
One study showed a 20% reduction in the risk of colon cancer and a 19% reduced risk of rectal cancer in those on HRT compared to those who are not (13).
Summary: Overall, when used appropriately and with bioidentical (micronized) progesterone specifically, risks of breast, endometrial, ovarian, and colon cancer are not increased with HRT, and may even be decreased in some cancers.
Conditions that Increase the Risk of Developing Cancer with HRT (and Without It)
The following comorbid conditions may pose an increased risk of cancer in those using HRT. It is important to discuss the benefit-to-risk ratio with a healthcare provider to determine the best course (14).
Prior history of hormone-sensitive cancer.
Personal or strong family history of breast/ovarian cancer.
Active liver disease
The liver processes and clears hormones, so in the presence of liver disease, it is harder for the body to metabolize and excrete hormones, allowing them to accumulate and increase cancer probability.
History of blood clots (DVT, PE) or clotting disorders (Factor V Leiden).
Although this risk is lower with the use of bioidentical rather than synthetic and transdermal rather than oral forms.
Cardiovascular disease or uncontrolled hypertension.
This risk is highest for oral estrogen, but instead decreases with the use of transdermal estrogen.
Obesity.
Obesity increases baseline estrogen levels and clotting risk, which is further escalated by the use of estrogen HRT.
What to Do If There’s A Family History of Cancer
According to a study by the University of Rochester Medical Center, “The risk of developing breast cancer due to taking hormone replacement therapy appears to be the same for women with a family history of the disease and without a family history.” (15)
Carriers of the BRCA gene who have gone through risk-reducing surgery may safely use HRT (37).
In general, guidelines state that all risk factors should be assessed and decisions made based on individual risks and potential benefits.
Factors to Consider:
Consider genetic testing, such as the BRCA gene, to assess risk.
Consider non-hormonal measures first.
Choose the lowest effective dose with the safest delivery method (combo HRT administered transdermally).
Consider estriol over estradiol for less potent activity.
Keep up with regular screenings and preventative care for breast, ovarian, and uterine health.
Consider other lifestyle factors such as menopausal symptoms, bone health, cardiovascular health, brain health, activity level, diet, and other conditions that relate to the overall benefit-to-risk ratio.
Do Benefits Outweigh the Risks?
The current understanding is that the benefits of HRT, of which there are many, outweigh the risks, which, when prescribed correctly, are very low.
Menopausal Symptoms (16)
HRT shows efficacy in:
Decreasing hot flashes, night sweats, vaginal dryness, and vaginal atrophy.
Increasing libido, vaginal lubrication, and orgasm.
Improving mood, sleep, and cognitive clarity.
Improving skin elasticity, hydration, and scalp hair growth.
Bone Health (17)
Estrogen and testosterone replacement are shown to improve bone density and decrease the risk of osteoporosis.
It does this by increasing bone building and decreasing bone breakdown.
HRT is considered as effective as osteoporosis medications at lowering the chance of broken bones in post-menopausal females.
Cardiovascular Health
Menopause increases the risk of heart disease, including hypertension, cholesterol, slower metabolism, increased visceral fat, and cardiovascular inflammation (18).
HRT significantly reduces all-cause mortality and cardiovascular disease (CVD), which other primary CVD prevention therapies, such as lipid-lowering, even fail to do (19).
Estrogen-based HRT was shown to improve cardiovascular biomarkers over time (20).
Lower cholesterol.
Reduced lipoprotein(a), a genetic variation associated with a higher risk of heart attack and stroke, for which there is currently considered to be no effective treatment!
Women on HRT show lower levels of atherosclerosis (plaque build-up in arteries), improvement in cholesterol, and increased blood flow (21).
Hormones appear to absorb free radicals in the blood that damage arteries and other tissues, thereby lowering blood vessel damage.
Women receiving estrogen were
30% less likely to die than those not on hormone therapies.
36% less likely to have a coronary calcium score above 399 (an indicator of severe atherosclerosis and high risk of heart attack).
20% more likely to have a coronary calcium score of zero.
Those with preexisting heart disease need to discuss with their doctor about stratified risk and benefits.
Brain Health
Some studies show that HRT used between 40 and 50 years old may protect against and reduce the risk of Alzheimer’s Disease and dementia (22).
The brain has a higher chance of being protected from dementia if HRT is started soon after menopause symptoms begin.
Estrogen-only HRT demonstrated a 32% lower dementia risk compared to those not using HRT if started within 10 years of menopause. Estrogen-progesterone therapy showed a 23% lower risk.
There is a positive association between HRT use and overall cognitive performance, including memory, processing speed, and executive functions (23).
It is worth noting that older studies showing an increased risk of dementia on HRT were done using synthetic hormones only, and specifically forms that are no longer used for HRT (progestins).
Metabolic Health
HRT is shown to reduce abdominal fat, insulin resistance, new-onset diabetes, lipid (cholesterol) levels, blood pressure, and pro-clotting factors in non-diabetic women. Insulin resistance, fasting glucose, and lipid levels are also reduced in diabetic women (24, 25).
Reduced visceral adipose tissue, BMI, and overall fat mass are shown on HRT, which is important for overall weight but also overall metabolic and organ health (26).
Longevity
Postmenopausal women with historical HRT use were biologically younger than those not receiving HRT (27).
Initiated in women under 60 years old, HRT significantly reduces overall mortality (19).
The same study noted that the magnitude and type of HRT-associated risks, such as breast cancer, stroke, and blood clots, are rare (less than 10 events per 10,000 women) and are not unique to HRT but are comparable to other medications. With this data, HRT is considered to have an excellent risk profile, especially compared to the benefits.
Summary: Overall, the benefits and risks of HRT can depend on your medical history, but for healthy menopausal females, it appears the benefits can substantially outweigh the risks and can blunt the onset of diseases that come with aging.
HRT After Cancer
Breast Cancer
Systemic (Whole Body) Estrogen/ Progesterone
Some studies show that estrogen/ progesterone HRT could increase the risk of recurrence in women with a history of breast cancer. However, other studies do not show an increased risk for breast cancer survivors compared to the general population (28). The studies that showed an increased risk used synthetic estrogen and progesterone, which could be the cause of the risk discrepancy (29).
Observational studies have even shown lower risk (30).
Because the risk of HRT and breast cancer recurrence in those with a prior history remains unclear, the decision to initiate HRT should be individual and discussed with a healthcare provider.
Those with risk-reducing surgery for the BRCA gene may safely use HRT (37).
Vaginal Estrogen
While systemic HRT is generally avoided, local vaginal estrogen does not appear to be associated with an increased risk of breast cancer recurrence, breast cancer-specific mortality, or overall mortality. It is therefore considered safe (31).
Testosterone (32, 33)
Testosterone is often forgotten about in women, but it is a crucial component of the HRT picture.
Studies show that subcutaneous testosterone alone or in combination with anastrazole (commonly used after breast cancer to prevent recurrence) reduced the overall incidence of breast cancer recurrence while effectively treating menopausal symptoms.
Testosterone and anastrazole implants placed in breast tissue with malignant tumors significantly reduced tumor size, further supporting the beneficial effects of testosterone.
Testosterone is therefore considered safe in breast cancer survivors and is an effective menopause treatment.
Uterine/ Endometrial, Ovarian, and Cervical Cancers
Systemic HRT
Those with a history of early-stage, low-grade endometrial cancers, epithelial and germ cell ovarian cancers, and early-stage squamous cell cervical, vulvar, and vaginal cancers may safely use HRT (34, 35, 36). The benefits are likely to outweigh the risks.
For those with advanced endometrial cancer, uterine sarcoma, and low-grade serous ovarian cancer, HRT is not recommended (34, 35).
Vaginal Estrogen
Vaginal estrogen is considered safe for uterine/endometrial, ovarian, and cervical cancer (37).
Other Non-Hormone-Dependent Cancers (36)
There is no clear research on HRT use in other forms of cancer. However, for survivors of non-hormone-dependent cancers, such as thyroid, skin, and colon cancer, systemic HRT may be considered, but is patient-specific and should be based on an individual benefit-to-risk assessment.
Those who have had risk-reducing surgery for Lynch syndrome can safely use HRT.
Summary: Vaginal estrogen and systemic testosterone are viable HRT options for those with histories of cancer. Other forms of HRT should be dependent on individual risks and discussion with healthcare providers. For those needing other ways to support menopausal symptoms without hormone therapy, check out this blog for alternative therapies.
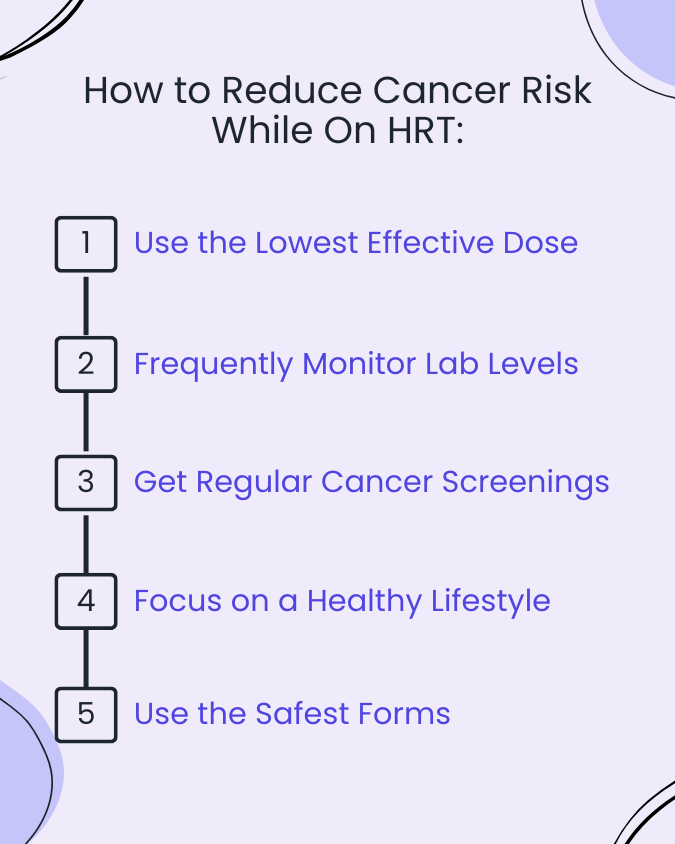
How to Reduce the Risks Associated with HRT
Monitoring
When initiating HRT, it is important to obtain serum hormone levels at baseline and every 8 weeks until a stable dose is achieved. Labs should be monitored every 3 to 6 months (annually if very well-controlled) for the duration of HRT use to ensure proper levels and prevent chronic overuse.
Dosing and Form Matters
Transdermal or subcutaneous forms of estradiol are preferred over oral to prevent the risk of clot, stroke, and elevated triglycerides and inflammatory markers.
Transdermal and subcutaneous forms bypass the liver, which allows lower risk, steady and controlled dosing, lower required dosing, and decreased stress on the liver (38).
Using the lowest effective dose supports menopausal symptoms and provides other systemic benefits, while reducing the risks from excess hormones.
Synthetic vs Bioidentical
While there is not much research on the use of bioidentical hormones, one synthetic hormone has clear negative effects: synthetic progestins. And its bioidentical counterpart, micronized progesterone, has clear positive benefits. Progestins are rarely used anymore; however, ensuring the correct form is used is still critical.
Lifestyle
Focusing on a healthy lifestyle reduces overall risk in every individual, with or without HRT. Maintaining a healthy weight, limiting alcohol, exercising, and eating a high-fiber diet all assist in metabolizing and excreting hormones, boosting overall health, and reducing disease risk.
Preventative Screenings
Regular breast exams and imaging (mammogram, ultrasound, or MRI) are important for catching breast irregularities and cancer early.
Pelvic exams (pap smears) screen for cervical cancer and can also be used to assess ovarian and uterine abnormalities to catch any concerns earlier.
Regularly monitoring blood pressure, lipids, and liver function ensures healthy heart and metabolic function.
Bottom Line: HRT does not cause cancer. The primary research that created fear around HRT and cancer was misrepresented and done using synthetic hormones that are no longer used (synthetic progestins). Hormones used in safe forms, with the lowest effective doses, appear to carry more benefits than they do risks, and possess many benefits for not just menopausal symptoms, but overall health and aging. Individual patients should be treated as just that: an individual. Talk with your healthcare provider to find the best options for you, and have peace of mind about the safety profiles of the treatment options available!
Resources:
https://www.sciencedirect.com/science/article/pii/S0378512223003584
National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Sciences Policy; Committee on the Clinical Utility of Treating Patients with Compounded Bioidentical Hormone Replacement Therapy; Jackson LM, Parker RM, Mattison DR, editors. The Clinical Utility of Compounded Bioidentical Hormone Therapy: A Review of Safety, Effectiveness, and Use. Washington (DC): National Academies Press (US); 2020 Jul 1. 7, The Safety and Effectiveness of Compounded Bioidentical Hormone Therapy. Available from: https://www.ncbi.nlm.nih.gov/books/NBK562865/
Abenhaim HA, Suissa S, Azoulay L, Spence AR, Czuzoj-Shulman N, Tulandi T. Menopausal Hormone Therapy Formulation and Breast Cancer Risk. Obstet Gynecol. 2022 Jun 1;139(6):1103-1110. doi: 10.1097/AOG.0000000000004723. Epub 2022 May 3. PMID: 35675607. https://pubmed.ncbi.nlm.nih.gov/35675607/#:~:text=In%20adjusted%20analyses%2C%20compared%20with,Menopause
Abenhaim HA, Suissa S, Azoulay L, Spence AR, Czuzoj-Shulman N, Tulandi T. Menopausal Hormone Therapy Formulation and Breast Cancer Risk. Obstet Gynecol. 2022 Jun 1;139(6):1103-1110. doi: 10.1097/AOG.0000000000004723. Epub 2022 May 3. PMID: 35675607.
Donovitz G, Cotten M. Breast Cancer Incidence Reduction in Women Treated with Subcutaneous Testosterone: Testosterone Therapy and Breast Cancer Incidence Study. Eur J Breast Health. 2021 Mar 31;17(2):150-156. doi: 10.4274/ejbh.galenos.2021.6213. PMID: 33870115; PMCID: PMC8025725.
Holtorf K. The bioidentical hormone debate: are bioidentical hormones (estradiol, estriol, and progesterone) safer or more efficacious than commonly used synthetic versions in hormone replacement therapy? Postgrad Med. 2009 Jan;121(1):73-85. doi: 10.3810/pgm.2009.01.1949. PMID: 19179815.
National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Sciences Policy; Committee on the Clinical Utility of Treating Patients with Compounded Bioidentical Hormone Replacement Therapy; Jackson LM, Parker RM, Mattison DR, editors. The Clinical Utility of Compounded Bioidentical Hormone Therapy: A Review of Safety, Effectiveness, and Use. Washington (DC): National Academies Press (US); 2020 Jul 1. 7, The Safety and Effectiveness of Compounded Bioidentical Hormone Therapy. Available from: https://www.ncbi.nlm.nih.gov/books/NBK562865/
Grodstein F, Newcomb PA, Stampfer MJ. Postmenopausal hormone therapy and the risk of colorectal cancer: a review and meta-analysis. Am J Med. 1999 May;106(5):574-82. doi: 10.1016/s0002-9343(99)00063-7. PMID: 10335731.
https://my.clevelandclinic.org/health/treatments/15660-bioidentical-hormones
https://theros.org.uk/information-and-support/osteoporosis/treatment/hormone-replacement-therapy/
Hodis HN, Mack WJ. Menopausal Hormone Replacement Therapy and Reduction of All-Cause Mortality and Cardiovascular Disease: It Is About Time and Timing. Cancer J. 2022 May-Jun 01;28(3):208-223. doi: 10.1097/PPO.0000000000000591. PMID: 35594469; PMCID: PMC9178928.
https://www.psu.edu/news/research/story/can-hormone-therapy-improve-heart-health-menopausal-women
https://www.cedars-sinai.org/blog/hormone-replacement-therapy-and-heart-health.html
https://www.urbanhealthtoday.com/post/starting-hrt-in-midlife-may-protect-women-from-dementia
https://www.frontiersin.org/journals/dementia/articles/10.3389/frdem.2024.1496051/full
HRT reduced aSalpeter SR, Walsh JM, Ormiston TM, et al. Meta-analysis: effect of hormone-replacement therapy on components of the metabolic syndrome in postmenopausal women. 2006. In: Database of Abstracts of Reviews of Effects (DARE): Quality-assessed Reviews [Internet]. York (UK): Centre for Reviews and Dissemination (UK); 1995-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK72592/
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2822953
https://www.ncoa.org/article/what-to-know-about-hormone-replacement-therapy-and-breast-cancer-risk/
Edey KA, Rundle S, Hickey M. Hormone replacement therapy for women previously treated for endometrial cancer. Cochrane Database Syst Rev. 2018 May 15;5(5):CD008830. doi: 10.1002/14651858.CD008830.pub3. PMID: 29763969; PMCID: PMC6494585.
Chambers LM, Herrmann A, Michener CM, Ferrando CA, Ricci S. Vaginal estrogen use for genitourinary symptoms in women with a history of uterine, cervical, or ovarian carcinoma. Int J Gynecol Cancer. 2020 Apr;30(4):515-524. doi: 10.1136/ijgc-2019-001034. Epub 2020 Feb 18. PMID: 32075898.
Mehta J, Kling JM, Manson JE. Risks, Benefits, and Treatment Modalities of Menopausal Hormone Therapy: Current Concepts. Front Endocrinol (Lausanne). 2021 Mar 26;12:564781. doi: 10.3389/fendo.2021.564781. PMID: 33841322; PMCID: PMC8034540.